Interviews
Interviews
Healthcare Culture in Japan vs. the UK: An Insightful…
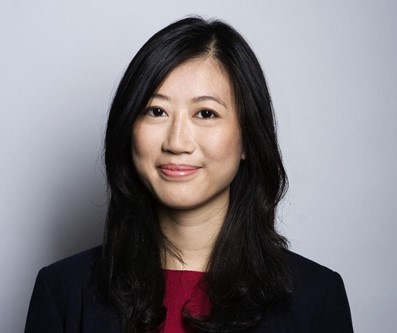
By Naoko Nomoto
With the effects of the Coronavirus still lingering on, how does each country respond in terms of medical care in such a pandemic? We felt this was a good opportunity to understand how we think about science and the underlying cultural differences that inform it. Tokyoesque’s Naoko Nomoto interviewed May Hagiwara, a Japanese nurse working in the UK, about the differences that exist between healthcare culture in Japan vs. the UK.

Thank you so much for speaking with me today. First of all, could you introduce yourself?
— No problem at all. I work as a registered nurse within the UCLH (University College London Hospital) Trust, in London. Originally, I graduated from a nursing university in Japan in 2015 and worked as a nurse for 2 years at St. Luke’s International Hospital (Gastrointestinal Medicine). However, I wanted to experience medical care outside of a hospital environment, so I left St. Luke’s to become a freelance nurse. Mostly, I worked as a local dispatch nurse and was involved in community nursing as well. I have also volunteered as a nurse in Sri Lanka for a short period of time.
After that I decided to go to the UK to experience medical care in other countries and to study medical English. I moved to London in June 2018. I chose to go to the UK because there were rumours that the country is making progress in terms of community nursing, and home care in general.
Initially, I worked as a Nursing Assistant at the same trust where I am still working. To transfer the Japanese nursing qualification to the UK, I had to pass three tests and it was a long process. After studying hard while I was working, I finally acquired the qualification to become a qualified nurse in March this year in the midst of this pandemic. It’s an extraordinary thing, but there are only three exam facilities across the UK providing OSCE (final test) for international nurses. Just before lockdown started, I had to fly all the way to Northern Ireland! This is one example of a British system that really doesn’t make sense if they want more nurses (laughs).
Currently, I am working full-time at the same hospital which specialises in neurosurgery. In the future, I hope to be involved in district (home-visit) nursing.
Thank you. I don’t think there are many people who have been involved in medical practice in various ways, and across two countries, England and Japan! What kind of work are you specifically doing now? And what kind of people do you work with in terms of ethnicity?
— The department I work in specialises in neurosurgery, so pre- and post-operative care for patients requiring brain /spine surgery are the main focus. In terms of people I work with, it’s a very international environment with staff originally from all over the world. It’s a great team, and everyone is treated with respect, not much of a hierarchy that I experienced in Japan. Regarding ethnicity, a high percentage of the staff we work with are Black or Asian.
The interesting thing is that I would say 90% of Asian nurses in my hospital are from the Philippines. Before the Coronavirus outbreak, there were nurses coming from the Philippines every month to take the OSCE and work here. There is a lot of support from the British government for Filipino nurses – they have a good support system, from providing examination preparations to supporting flight fares. I was lucky to join the exam prep with them.
In the Philippines, the level of English education is excellent and all education including nursing is provided in English as well. They are also very hard working! I think for this reason, it makes their transition into the UK workforce smooth, hence the support.

It’s well known that there are not enough nurses in Japan as its society continues to age, but I can’t imagine Japan is doing similar initiatives to encourage foreign workers in Japan.
— Exactly, and unfortunately Japan doesn’t do this at all. Japanese language is certainly one barrier, but as the young population shrinks, more and more foreign workers will be needed in the future in Japan.
What makes this possible is the position of “nursing assistant” or “healthcare assistant”, the number of which is increasing all over the world. This is a position that does not strictly exist in Japan. The Nursing Assistant in the UK, literally “supports” the staff nurse and is in charge of routine tasks such as taking vital signs (blood pressure etc.), measuring blood sugar level, the personal care of patients and so on. In Japan, qualified nurses do all of these clerical duties. This, therefore, cuts into time that could be spent doing more specialised work. Nursing assistants are now commonplace in Australia, the US and the UK and many other countries. It’s a position I would like to see introduced in Japan as I believe it can be very beneficial.
If this position were introduced, I can see the burden on staff nurses would be considerably reduced. Now I would like to ask you, what is the biggest difference between healthcare culture in Japan vs. the UK?
— In a nutshell, the UK is free and Japan is restricted. For example, in the UK, there is a strong idea that a patient’s will is absolute. They have more dignity and freedom of choice. From the treatment method to the types of meals they receive at the hospital, it’s primarily up to the patient. This all seems good, but too much choice for the patients can be questionable as well. For instance, I was surprised the first time I was in charge of patient mealtime in the UK. Each person is given a menu, and there are even dishes with low nutritional values such as Fish and Chips and Cottage Pie. There’s even big bowl of desserts! And they can choose whatever they like.
That sounds very much like a pub, doesn’t it? (laughs). So, what’s it like in Japan?
— In Japan, we provide 100% balanced meals with nutritional values calculated by dietitians. Depending on the patient’s health condition, different versions are automatically applied such as; low protein food for patients with kidney failure, food with lower sugar for diabetic patients, and paste versions for those with swallowing difficulties. Besides, they are usually all handmade from scratch! But you have to eat it, or you won’t get another meal. Japan is far ahead in terms of healthy and delicious meals, but I think there are too few options compared with the UK. As Japan becomes more international, it must also respect various dietary requirements, such as gluten-free, vegan, and religious restrictions.
In Japan, does the lack of food choices reflect the overall attitude of medical services too?
— Patients in Japan still feel that “doctors know best” and they are expected to comply with what the healthcare professional advises. On the other hand, In the UK “Informed Consent” is done properly. This is fundamental for patients, in the sense that they are “informed” of the risks and benefits of procedures and give their “consent” after understanding the information they’ve been told. Although informed consent is done in Japan as well, it is mainly for choices in treatment such as surgery and not embedded in every little communication like it is in the UK.
For example, when taking someone’s blood pressure in Japan, we tend to say “okay, it’s time to take your blood pressure,” whereas in the UK, nurses are always expected to explain to the patient any procedure they may need and seek the patient’s permission. Even if it’s something as mundane as taking blood pressure.
Of course, not all choices patients make are correct, so for me it’s the healthcare professionals’ job to strike a balance about where to respect their choice and where to explain further. Therefore, if a patient rejects a vital treatment, I will make sure the patient is making the choice based on the right information and knowing the risks for their health. In Japan, I think it’s rare for a patient to refuse the recommended treatment. This illustrates the sort of fundamental cultural difference.
— There is a lot to say about the political side for the response to the virus, but in terms of the medical field, I think NHS hospitals did their best despite the high proportion of Coronavirus patients. My trust had a big role to play and helped many patients, however there are a few things Japan and UK could learn from each other.
When the number of Coronavirus patients surged in the UK, we had a massive shortage of staff because those with symptoms had to stay away for two weeks to self-isolate. In my ward, many general operations were postponed, so some of us were deployed to the Coronavirus ward to help out. We also braced for the worst and got ready for people who are usually managers, specialist nurses, or seniors to come and help general staff nurses for the first time in decades. Nursing students came into the workforce too. Even general nurses had training for helping ICU nurses. So there was good preparation of manpower which Japan didn’t have if there was a bigger spike.
However, there is a possibility that in the UK, the virus may have been passed on by some of the asymptomatic nurses/patients to patients within the hospital in the early stages. In Japan, despite having only a few cases, all nurses in any setting were required to wear masks from the beginning, which was introduced later in the UK. Most nurses in Japan wore masks almost everyday anyway, even before the outbreak, so they’re used to it.
Also, Japanese nurses were not allowed to talk during lunch breaks and had to maintain social distancing during the outbreak. Furthermore, a few nurses were appointed to take care of Coronavirus patients who were being cared for in negative pressure side rooms and were isolated from other patients or other nurses. This must have been stressful, but may have prevented transmissions within a hospital. As for the UK, nurses took turns taking care of patients to reduce stress and were provided with mental support.
I believe this was necessary despite some risks as there were too many cases in the UK at once. In terms of masks, I understand there was a shortage but there is too little etiquette and lack of prevention around infectious diseases in the UK. In Japan, there is a wide-spread understanding that when flu season comes around, everyone wears a mask to prevent the spread, not to mention that washing hands and gargling is an everyday routine. Even with a normal flu, if one has symptoms, it’s mandatory to self-quarantine and not go to school or work.
On the whole, I think Japan’s everyday hygiene in addition to the restrictive and compliant culture helped to stop the virus from spreading, but it’s hard to compare as the number of cases were so different.

I see. And in the UK there was incredible information that certain ethnic groups had a high fatality rate, but how is it in reality?
— I can’t really say if there is a higher mortality rate due to the genetic difference as they’re still trying to find out the reason. It could well be to do with the high proportion of key workers who had no choice but to go out are people of colour such as bus drivers, delivery agents, shop salespeople, and so on. So, it stands to reason that they were at much higher risk of infection. I don’t believe there is a discrimination such as not treating them well because of their race. Healthcare professionals treat people equally no matter their race or background.
Another thing to note is, how people with underlying health conditions are vulnerable to Coronavirus. It might be the case that some ethnic groups are more prone to these illnesses because of food or cultural differences? I remember when I volunteered in Sri Lanka, we found many people had diabetes and one reason was the high sugar intake in the cups of tea that they drink so many times a day.
Talking about underlying chronic illnesses, the degree of contraction is higher in the UK than in Japan. For example, I was surprised at how many people in the UK have diabetes. When I gave insulin to a patient in Japan, I only saw a maximum of 18 units. But since I came here, I’ve seen some people needing a maximum of 68. It’s possible that people with poor dietary education and those on low income have difficulty maintaining a proper diet.
Interesting. As one of the UK’s key workers, what’s the work-life balance like for nurses here?
— British nurses have a great work-life balance! In Japan, shifts of 8 hours per day and 16 hours at night are common. When I tell my UK colleagues that, many say “Isn’t that illegal?” It sure feels like it! It’s understandable that such long working hours may lead to incidents and other issues in Japan. On the other hand, in the UK, there are 12-hour day shifts and 12-hour night shifts as well as much longer annual leave. There is a proper awareness around “protecting the health of nurses.” I feel that there are various services in place that nurses can access, and these are well protected. That is why I can continue to be a nurse. To be honest, I think Japan should value and protect their nurses more.
— Well, in terms of technology, I think electronic medical records are more advanced in Japan. Even the London hospital I work for has only recently adopted them. When I came to the UK, it was still paper charts. If Japan could provide something to the UK, it would be preventive medicine and public health strategies to maintain patients’ health. But above all, I think education about food and nutrition is one of Japan’s key strengths. There’s a lot of demand for this in the UK, so I hope that aspect can grow in the future.
On the contrary, what Japan could adopt from the UK are some manual handling equipment such as hoists or “Sara Stedys”. It’s a great way to move a bedridden patient into a chair and it prevents nurses from hurting their backs while encouraging patients out of bed. It benefits both nurses and patients. Sitting bedridden patients is an important opportunity to open the lungs and train the breathing muscles.
Another important aspect that can be learned from the UK is education about diversity. As Japan becomes more international, there needs to be an understanding of different cultures and religions in healthcare settings. Safeguarding is another aspect Japan needs to learn from the UK. Supporting people in vulnerable groups and protecting dignity needs to be improved upon.
Biography: May Hagiwara
May Hagiwara was born in 1992. She graduated from st. Luke’s International University is Tokyo in 2015 and worked at St. Luke’s International Hospital. After gaining experience as a freelance nurse, focusing on community nursing, she moved to England in 2018 to study medical care in other countries as well as to study medical English. While working as a nursing assistant at University College London Hospital (UCLH), she earned a British national nursing qualification during the Coronavirus outbreak. She is currently working as a staff nurse at the same hospital.
On the subject of healthcare culture in Japan, why not check out our previous blog post all about agetech in Japan? If you’re interested in conducting research on the healthcare sector let us know.
We’ll be adding more healthcare-related articles on Japan in the future, so keep checking back or follow us on LinkedIn, Facebook or Twitter to get notified about our latest posts!